10年疗效观察结果显示HTO结合CR对膝内翻伴严重骨关节炎患者是理想治疗选择
2019-01-26 文章来源:骨科在线 点击量:1334 我要说
来源:304关节学术
译者:张轶超
整理:骨科在线
来自德国的Schuster P等人在线发表于《Am J Sports Med》杂志的一项研究显示,对于内翻膝伴严重内侧骨关节炎的病例,胫骨高位截骨(HTO)结合软骨修整术(CR)是一个理想的治疗选择。
对于早期膝内翻伴内侧骨关节炎的患者,尤其是年轻患者,HTO是一个理想的选择。但是应用此术式治疗严重骨关节炎患者的相关数据是有限的,而且由于新的内植物的使用,更缺乏长期观察数据结果。因此研究人员旨在评估内翻膝伴严重内侧骨关节炎(Kellgren-Lawrence 3和4级)的患者接受HTO结合CR(软骨修整加微骨折)的生存率及效果,并试图分析影响效果的潜在因素。
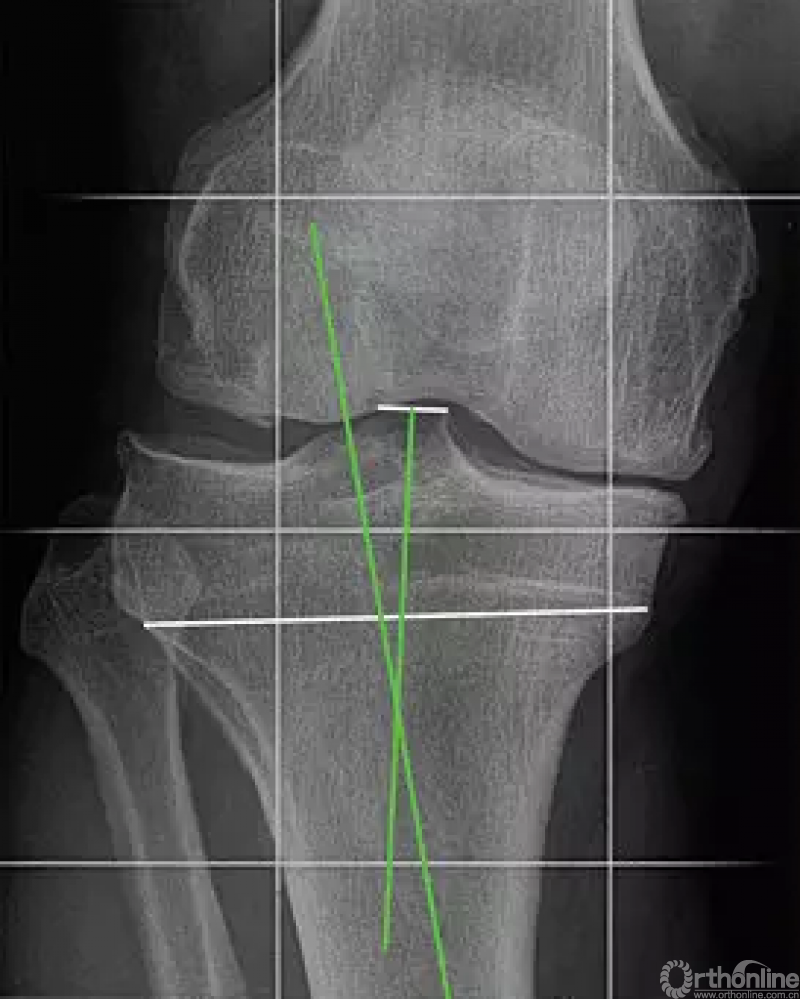
根据Bonnin和 Chambat的方法测量胫骨内翻角(TBVA)。测量方法是胫骨髁间棘的中点和残存的骨骺线的中点的连线与胫骨机械轴所成的夹角
作者设计一项前瞻性研究,观察了从2005年9月到2008年12月的所有接受HTO(角钢板内固定)结合CR手术的患者,观察了其生存率((Kaplan-Meier法,不需要行关节置换的患者数量) 和功能效果(主观国际膝关节资料委员会[IKDC]评分)。通过记录去除钢板时软骨退变的情况、胫骨内翻角(TBVA)、术前和术后机械胫骨内侧近端角(MPTA)及术后整体力线来进行结果分析。
结果显示,研究共纳入79膝(73名患者,平均年龄50.9±7.6岁)。随访达到10.0±1.2年(8.3-12.1年)比例为90%。术前和术后的股骨胫骨机械轴成角分别为内翻9.6±3.0°和外翻0.6±2.7°。术后10年的生存率为81.7%(95%可信区间为72.5%-90.9%)。主观IKDC评分有明显改善,从术前的44±11分升高到术后1年时的70±13分,3年时的66±15分,5年时的66±15分,10年时的65±17分(与术前比较任何时间段的P<0.001)。软骨退变明显的和术前IKDC评分低(<40分)的患者的生存时间比较短。最终随访时发现术前TBVA角度较大的效果较好,而MPTA矫正过度(>95°)的则功能效果欠佳。
作者表示CR手术在治疗中处于什么地位还不太清楚,同时尽管过度矫正MPTA获得了好的早期结果,但长期功能相对欠佳。
原文摘要:
Ten-Year Results of Medial Open-Wedge High Tibial Osteotomy and Chondral Resurfacing in Severe Medial Osteoarthritis and Varus Malalignment
BACKGROUND:
High tibial osteotomy (HTO) is a widely used treatment option for medial osteoarthritis and varus malalignment, especially in young patients with early osteoarthritis. Limited outcome data are available for this procedure in severe osteoarthritis, and no long-term data are available using newer implants.
PURPOSE:
To determine survivorship and functional results of medial open-wedge HTO combined with a chondral resurfacing (CR) procedure (abrasion plus microfracture) in severe medial osteoarthritis (Kellgren-Lawrence grade 3 and 4) and varus malalignment. Furthermore, factors that potentially influence the outcome were analyzed.
METHODS:
From September 2005 to December 2008, all cases of HTO (fixation with an angular-stable internal fixator) combined with CR were prospectively surveyed with regard to survival (Kaplan-Meier-method, not requiring arthroplasty) and functional outcome (subjective International Knee Documentation Committee [IKDC] score). Cartilage regeneration at the time of hardware removal, tibial bone varus angle (TBVA), pre- and postoperative mechanical medial proximal tibial angle (MPTA), and postoperative alignment were analyzed with regard to the result.
RESULTS:
Seventy-nine knees were included (73 patients; mean age 50.9 ± 7.6 years). The follow-up rate was 90% at 10.0 ± 1.2 years (range, 8.3-12.1 years). Pre- and postoperative mechanical tibiofemoral axis were 9.6° ± 3.0° of varus and 0.6° ± 2.7° of valgus, respectively. Survival rate was 81.7% (95% CI, 72.5%-90.9%) at 10 years. Subjective IKDC score significantly improved from 44 ± 11 preoperatively to 70 ± 13 at one, 66 ± 15 at three, 66 ± 15 at five, and 65 ± 17 at ten years ( P < .001 at any point of follow-up). Poor cartilage regeneration and low preoperative IKDC score (<40) were associated with decreased survival. High preoperative TBVA was associated with better and an overcorrected MPTA (>95°) with inferior functional outcome at final follow-up, respectively.
CONCLUSION:
Even in cases of severe medial osteoarthritis and varus malalignment, HTO in combination with a CR procedure is a good to excellent treatment option. The role of the CR procedure remains unclear. Although good results are obtained with overcorrected MPTA, long-term functional outcome is inferior.
文献出处:
Schuster P, Geßlein M, Schlumberger M, Mayer P, Mayr R, Oremek D, Frank S, Schulz-Jahrsdörfer M, Richter J. Ten-Year Results of Medial Open-Wedge High Tibial Osteotomy and Chondral Resurfacing in Severe Medial Osteoarthritis and Varus Malalignment. Am J Sports Med. 2018 May;46(6):1362-1370. doi: 10.1177/0363546518758016. Epub 2018 Mar 28.



 京公网安备11010502051256号
京公网安备11010502051256号