钩突的发生与发展及其临床意义
2020-02-28 文章来源:海军军医大学第二附属医院骨科脊柱一病区 孙柏峰 刘洋 我要说
钩突普遍存在于C3-C7椎体上终板的外侧缘并与上位椎体下终板的外侧缘共同形成钩椎关节,也被称为luschka关节,是人体重要的解剖学结构[2][3][4][5]。虽然缺少关节囊的包裹,但钩椎关节既有协同椎间盘、关节突关节等完成颈椎运动的作用,同时还具有维持颈椎稳定性的作用[6]。除颈椎椎体具有钩突这一结构外,Tulsi 等发现在部分人群中钩突也可存在于T1-T2椎体的外上缘[7]。目前对钩突及钩椎关节的研究不仅包含解剖学、影像学还包括了病理学、生物力学等等。本文通过对现有文献的回顾,综述钩凸的发生与发展及其临床意义,希望对临床治疗由于钩椎关节退变而引起的神经根型颈椎病提供参考。
钩突的发生及钩椎关节的形成
人体绝大部分的关节在胚胎第7-8周逐渐发育成形,到了胚胎第10-11周,人体逐渐形成滑膜组织。而钩椎关节的发育则相对迟缓,首先,钩突在胚胎3-4个月时才逐渐发育。胚胎成熟之后,钩突与上一位椎体之间的并未形成明显的滑膜组织,其间充满了疏松的纤维组织和血管[8](图1)。钩突在4岁左右时开始向上生长。到了8岁左右,随着钩突的变高、变宽,椎间盘两侧后方逐渐形成一裂隙。20-35岁时,钩突两端后外侧的裂隙逐渐向中间汇聚,并在45岁左右时将椎间盘分成上下两部分[9][10]。
目前关于这一滑膜裂隙的形成原因尚不明确,Prescher等人认为其形成的原因可能与颈椎的运动及颈椎生理前凸的形成有关[11]。而Mercer等则认为这一结构的形成是由于颈椎运动时椎间盘受力导致,并配合颈椎完成轴向旋转运动[12]。Orofinod等人发现,在成人颈椎当中,原本存在于钩突与上位椎体之间的疏松纤维组织及血管被纤维软骨及新生骨组织所代替。这一改变也使钩突被认为是由于随着年龄的增长而出现的一种退变现象[9]。在颈椎退变过程中,由髓核脱水、椎间盘高度丢失等因素导致钩突与上一位椎体直接接触面积增大或承载压力变大,而在钩突周围出现骨赘。引起椎间孔狭窄,神经受压,从而出现颈椎病的临床表现[13][14]。
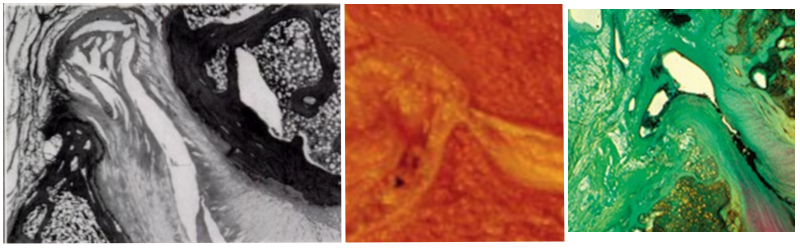
图1.切片可见钩突表面的滑膜组织[8]
钩突及钩椎关节的解剖
钩突常见于C3-C7椎体的外上缘,并与上一位椎体的下终板共同构成钩椎关节。同时,钩突的后缘则与上一位椎体的后下缘构成颈椎椎间孔的前壁,有着重要的解剖学意义[15][16]。目前,大部分国外研究认为C3-C7钩突的高度、宽度及长度呈逐渐增加趋势[17]。但也有文章指出C7椎体的钩突高度明显小于C6椎体。
而从宽度来看,C5椎体的钩突略窄于C4。也有学者认为,钩突的长度方面,C6椎体的钩突明显长于C7[18][19][20][21]。造成测量结果的差异可能与测量方法的不同及尸体样本的差异有关,也使得目前所获得的测量结果无法形成客观规律,且目前大多数钩突解剖学研究主要以高加索人种为主,缺少对亚洲人群的研究。近年来,Zhu等人对136位无颈椎退行性改变的中国人的680对钩突进行了CT三维重建的形态学研究,发现成年男性钩突略大于女性,C6两侧钩突的长度均长于C7,这也与一些国外文献相吻合。
由于两侧钩突后缘之间的距离对减压范围有着重要的指导意义,该研究还对这一数值进行了测量统计。测量发现C3椎体两侧钩突之间距离最小。在男性中,C3椎体两侧钩突后缘距离约8.87±1.31毫米,女性为8.54±1.18毫米。C6体两侧钩突之间距离最大,男性约15.41±1.51毫米,女性约13.37±1.23毫米。这一结果也与Kim等人在韩国人群中的颈椎研究相似[22][23]。
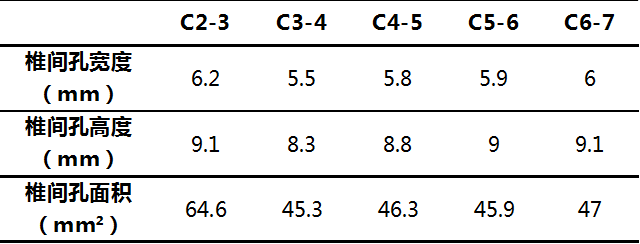
此外,在颈椎屈伸活动过程中,椎间孔宽度会发生一定的改变。钩突增生通常导致椎间孔狭窄,引起神经根受压,导致患者出现神经根型颈椎病症状[24][25][26][27]。Panjabi等人通过对文献的回顾,总结出正常椎间孔的宽度、高度及面积(图2.;表1.)。并指出,对于颈椎管狭窄的人群更容易出现神经根受压的情况,且下颈椎的背根神经节受压风险更高,特别是在遭受外伤的情况下[28][29]。Hong等人通过对伴有退行性改变的颈椎标本进行MRI及CT测量,发现C5-6椎间孔前后径最窄,约为3.5毫米。而Humphreys等人对C5-6椎间孔前后径的测量结果更为狭窄,约为2.4毫米。两组研究得出的数据均明显小于正常颈椎椎间孔的前后径[30][31]。
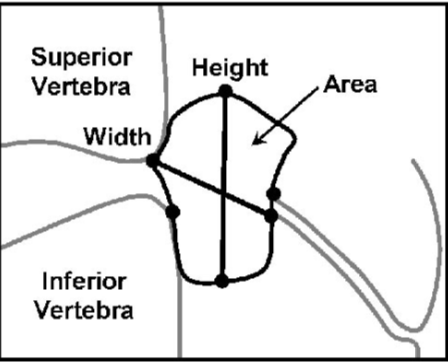
图2.Panjabi等人提出的椎间孔宽度及高度的测量方式
表1. Panjabi等人总结的正常椎间孔宽度、高度及面积
钩突与钩椎关节的功能
钩突是构成颈椎椎间孔前壁的重要组成部分,Yamazaki等人通过对200例颈椎病患者进行CT检查发现,其中198例颈椎间盘突出都是中央型和旁中央型,只有2例椎间盘侧方突出发生在C7-T1。这是因为钩突常位于颈椎椎体上终板的外缘,可以防止椎间盘向侧方突出[32]。而T1椎体通常缺少钩突这一结构,所以C7-T1更容易出现椎间盘向侧方突出的情况[33]。
除此之外,钩椎关节还是颈椎运动过程中重要的结构。颈椎的活动并不是由单一结构引起的屈伸变化,而是合并了钩椎关节活动的耦合运动,可以将颈椎的活动视为椎间盘与双层钩椎关节及双侧关节突关节共同作用的结果[34]。文献报道,切除C5-6钩突后,颈椎的屈、伸、侧曲及旋转活动度分别增大6%、5%、16%及24%。这也说明钩椎关节同时是限制颈椎过度活动重要结构[35]。钩突在维持颈椎稳定性方面也发挥着重要作用。通过对解剖及形态学的研究发现,由于下颈椎钩突的形态通常表现为前窄后宽,所以钩突的后半部分在维持颈椎稳定中起到了主要作用。且在颈椎背伸活动过程当中,C3-4的钩椎关节承担了颈椎48%-60%的稳定性[36][37]。
另一方面,颈椎在旋转的同时,运动方向同侧的钩椎关节间隙变窄,而对侧钩椎关节则逐渐分离。在颈椎旋转运动过程当中,C4-5、C5-6表现出良好的活动度。随着旋转角度的增加,C2-3、C3-4、C4-5钩椎关节的接触面积逐渐增大,而C5-6、C6-7钩椎关节的接触面积反而逐渐减小。这种现象也使得应力集中在更小的接触面积上,可能是导致C5-6、C6-7钩椎关节更容易发生退变的主要因素。颈椎的活动同时也会导致椎间孔面积的改变。当颈椎屈曲时,椎间孔面积会略增大。而背伸时,椎间孔面积则相应的减小。背伸20°时,椎间孔面积减小约10%;至30°时减小约13%。除椎间孔面积的改变之外,在颈椎及手臂活动的同时,神经根所承受的压力也在发生变化[38][39]。
钩突与钩椎关节的病理改变及治疗方式
钩突变得扁平,周围骨赘形成导致椎间孔狭窄是颈椎退变的主要表现之一。同时也提示该节段颈椎稳定性欠佳。由于骨赘压迫神经根而引起的症状通常需要手术治疗才能得到缓解[40][41][42]。此外,钩椎关节结构的不稳定及功能异常也被认为是引起神经根型颈椎病的重要因素[43][44][45]。通常情况下,神经根在椎间孔的下1/3通过,钩突的顶点一般位于神经根的上方。但随着髓核组织的脱水,椎间隙高度的丢失,钩突变得扁平并在周围形成坚硬的骨赘,导致椎间孔狭窄,并对神经根造成压迫[46]。
不仅如此,Brismée等人通过对2具高龄尸体的钩椎关节病理学研究发现,退变的钩椎关节表面含有P物质(SP)、神经肽Y(NYP)及降钙素基因相关肽(CGRP)等疼痛相关递质,这也说明退变的钩椎关节可能是引起颈部不适潜在因素[47]。此外,钩突还可能导致患者出现斜颈。2003年Maineg报道了一例15岁急性斜颈的男性患者出现急性斜颈,无法旋转及朝向一侧屈颈。通过磁共振成像显示右侧C2-C3钩椎关节内的出现高信号。作者推测,突然的外力可能导致钩突间隙的纤维结果急剧裂开引起水肿,导致钩椎关节内出现水肿样的高信号,从而引起患者出现避免疼痛的被迫体位。
对于钩椎关节退变导致的神经根型颈椎病,术中是否应该完整切除退变严重的钩突骨赘尚存争议。1955年Robinson和 Smith首次提出颈前路减压植骨融合内固定术(anterior cervical discectomy and fusion,ACDF)来治疗颈椎病,但文中并未提及对钩突骨赘的完整切除[48]。此后,Cloward提出所有致压因素都应被去除的观点,其中就包括了对神经根形成卡压得钩突骨赘[49]。但Robinson坚持认为手术切除增生的钩突骨赘与术后症状的改善之间并没有必然联系,且脊柱稳定性重建之后,骨赘可逐渐缩小甚至消失[50]。
时至今日,支持切除钩突的学者认为,这样做可以更快的让症状得到恢复且获得更好的临床效果[51][52][53][54]。而反对切除钩突的学者则认为,单纯且充分的椎间隙减压、椎间盘切除同样可以获得良好的临床效果。且神经根及椎动脉与钩椎关节结构紧密。切除退变的钩突骨赘可能会增加神经根及血管损伤的风险,并认同Robinson之前提出的稳定重建之后,骨赘可消失的观点[55][56][57]。
据文献报道,虽然ACDF术引起血管损伤的概率只有0.3%-0.5%,然而一旦出现椎动脉等颈部血管的损伤,结果往往十分严重,可能会导致脑供血不足,严重的损伤甚至会引起患者的死亡[58][59][60][61][62]。对此,Park等人通过对椎间孔的影像学研究发现,如果手术过程中医生需要对钩椎关节进行减压,从椎体的中线向两侧减压不超过13毫米,可以在一定程度上避免对椎动脉的损伤并获得最大程度的减压范围[63]。(图3.)
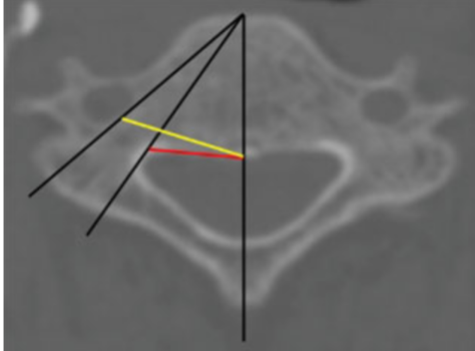
图3.红线表示颈前路手术的安全减压范围,黄线为中线至横突孔的距离
为了探讨直接对钩椎关节减压是否有必要,Shen等人对比了ACDF术中切除钩突组与单纯切除椎间盘组之间的临床效果及融合情况,发现术中无论是否切除钩突,术后患者颈痛症状均得到明显改善。此外,充分的撑开椎间隙可以间接的增大椎间孔的高度及宽度。
但Shen等人认为,虽然有内植物的支撑,但钩突减压后,椎间孔的前壁结构遭到破坏造成的稳定性降低可能会影响融合的速度及融合情况[64]。即便如此,如果为了获得钩椎关节的间接减压而选用过大的植入物同时也会导致颈椎屈伸活动度的减小[65]。这也是手术治疗钩椎关节退变所面临的矛盾之一。
除ACDF术外,颈椎显微技术、椎间孔镜等微创技术的提出,也为手术医生对钩椎关节进行减压提供了另一种途径。但无论是颈椎椎间孔镜技术还是Salvatore等人提出的斜方入路去除钩突增生骨赘的方法,虽然均可获得良好的减压范围,但目前无法实现椎体间融合[66]。这些术式在去除致压因素的同时也破坏了椎间孔的结构,在没有融合的情况下增加了颈椎的不稳定性[67]。不仅如此,Jing等人通过对52例人工椎间盘术后患者的5年随访中得出结论,钩椎关节骨化可能是引起患者术后出现轴性痛的危险因素[68]。
近年来,韩国学者提出应用高速动力磨钻对钩突进行完整切除,可以获得较为满意的临床效果。但高速动力磨钻因其机械减压的原理,容易引起硬膜及神经的损伤。超声骨刀应用于脊柱外科以来,因其热效应及气化效应,使得脊柱外科医生在对骨组织进行精确切除的同时,可以有效的避免血管及神经的损伤。但过度暴露钩椎关节,可能引起术中牵拉气管的时间延长,从而导致吞咽困难等发生。
值得注意的是,对于颈椎外伤的病人同时应该注意钩椎关节是否存在移位及钩突骨折,由于钩突在X线片上显影有一部分重叠,因此对于可疑损伤的病例应行进一步检查,否则容易造成漏诊。在严重的头颈部损伤中,通常伴有钩椎关节的脱位。Jonsson等人通过对在车祸中发生颅骨骨折的患者进行研究发现,绝大部分车祸导致的颅脑损伤患者均伴有不同程度的钩椎关节脱位,且大部分脱位为多节段双侧损伤。因此Jonsson等人得出结论,认为这类车祸导致轮脑外伤的患者极易合并钩椎关节的损伤,有时甚至仅有钩椎关节的脱位及椎间盘的破裂,而不伴有颈脊髓的损伤[69]。Yetkin等人通过对颈椎骨折的病人进行CT检查发现,大部分颈颈椎骨折的病人都伴有钩椎关节的脱位[70]。
因此,对因车祸导致的颅脑损伤的患者来说,应该仔细检查,避免遗漏颈椎钩椎关节损伤的情况。
小结
综上所述,近几年对钩椎关节的研究呈逐渐增加的趋势。越来越多的学者开始关注由于钩椎关节退变而引起的神经根型颈椎病。对于钩椎关节是否可以被称为真正意义上的关节一直存在争议。但通过对文献的回顾,不难发现,钩椎关节不仅是阻挡颈椎间盘向侧方突出的骨性结构,同时还是颈椎活动过程中必不可少的部分,并有着维持颈椎稳定性的重要意义。
对于经典的ACDF术,切除钩椎关节虽然可以获得较为满意的临床效果,但同时延长了手术时间并增加了并发症发生的风险。因此,在术中不必常规切除钩椎关节,应视具体情况而定。如若需要对钩椎关节进行减压,术前也应完善影响学检查,排除患者椎动脉走形异常及神经根发育异常的情况。对于行颈椎人工椎间盘置换术的患者,术前应仔细评估患者的影像学检查,对于术前已经伴有钩椎关节退变的患者,应谨慎选择此种手术方式。
因为颈椎人工椎间盘置换术本身保留了手术节段的活动度,术中如果为了获得充分的减压而过多切除钩突会引起颈椎稳定性的降低,且钩椎关节骨化可能是该手术方式术后出现轴性疼痛的危险因素之一。对于钩椎关节退变引起的神经根型颈椎病,椎间孔镜虽然可以更为精准的去除增生的钩突,但能否维持颈椎稳定性同时也是学者们一直争论的焦点,且术中操作不当甚至会加速椎间盘组织的退变过程。因此,还应有更长期的随访结果及统计分析来佐证。
目前,大多数文章集中在钩突的解剖学及生物力学研究,尚缺少高质量的临床随机对照研究。希望未来可以有更多关于钩椎关节退变与颈痛之间关系的基础研究及高质量的临床研究,从而提出治疗由于钩椎关节退变造成的神经根型颈椎病的临床依据。
参考文献
1. Rathcke. Zur normalen und pathologischen Anatomie der Halswirbelsäule[J]. Deutsche Zeitschrift für Chirurgie,1934,242(11-12).
2. F. Walcker. Die Hautarterien des menschlichen Körpers[J]. Deutsche Zeitschrift für Chirurgie,1912,117(3-4).
3. SPURLING RG, SEGERBERG LH. Lateral intervertebral disk lesions in the lower cervical region. Journal of the American Medical Association, 1953, 151(5), 354.
4. Browne Kenneth M. The anatomy, spatial relationships, and role of uncovertebral articulations as the source of posterolateral cervical cartilage sequestrations.[J]. Journal of Neurosurgery: Spine,2010,12(3).
5. Tubbs R Shane,Rompala Olivia J,Verma Ketan,Mortazavi Martin M,Benninger Brion,Loukas Marios,Chambers M Rene. Analysis of the uncinate processes of the cervical spine: an anatomical study.[J]. Journal of Neurosurgery: Spine,2012,16(4).
6. Nagamoto Y1, Ishii T, Iwasaki M, Sakaura H, Moritomo H, Fujimori T, Kashii M, Murase T, Yoshikawa H, Sugamoto K. Three-dimensional motion of the uncovertebral joint during head rotation. J Neurosurg Spine, 2012,17(4), 327-333.
7. Tulsi, R. S., Perrett, L. V. The anatomy and radiology of the cervical vertebrae and the tortuous vertebral artery. Australasian Radiology, 1975, 19(3), 258-264.
8. Orofino, C., Sherman, M. S., Schechter, D. Luschka's joint-a degenerative phenomenon. Jbjs, 1960, 42(5), 853-858.
9. Bland J H,Boushey D R. Anatomy and physiology of the cervical spine.[J]. Seminars in arthritis and rheumatism,1990,20(1).
10. Taylor, J., Twomey, L., Bo, L. Contrasts between cervical and lumbar motion segments. Critical Reviews in Physical & Rehabilitation Medicine, 2000, 12(4), 28.
11. Prescher A. Anatomy and pathology of the aging spine.[J]. European journal of radiology,1998,27(3).
12. Mercer S,Bogduk N. The ligaments and annulus fibrosus of human adult cervical intervertebral discs.[J]. Spine,1999,24(7).
13. Dvorak Jiri,Sutter Martin,Herdmann Joerg. Cervical myelopathy: clinical and neurophysiological evaluation.[J]. European Spine Journal,2003,12 Suppl 2.
14. Resnick D. Degenerative diseases of the vertebral column.[J]. Radiology,1985,156(1).
15. LYON,ERNST. Uncovertebral osteophytes and osteochondrosis of the cervical spine. Jbjs,1945, 27(2), 248-253.
16. Kotani Y,McNulty P S,Abumi K,Cunningham B W,Kaneda K,McAfee P C. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine. A biomechanical study.[J]. Spine,1998,23(14).
17. Hartman Jeffrey. Anatomy and clinical significance of the uncinate process and uncovertebral joint: A comprehensive review.[J]. Clinical anatomy (New York, N.Y.),2014,27(3).
18. Russo Vittorio M,Graziano Francesca,Peris-Celda Maria,Russo Antonino,Ulm Arthur J. The V(2) segment of the vertebral artery: anatomical considerations and surgical implications.[J]. Journal of Neurosurgery: Spine,2011.
19. Milne N. The role of zygapophysial joint orientation and uncinate processes in controlling motion in the cervical spine.[J]. Journal of anatomy,1991,178.
20. Peter Petty. Surgical Anatomy of the Anterior Cervical Spine: The Disc Space, Vertebral Artery, and Associated Bony Structures[J]. Neurosurgery,1997,41(1).
21. Lu J,Ebraheim N A,Yang H,Skie M,Yeasting R A. Cervical uncinate process: an anatomic study for anterior decompression of the cervical spine.[J]. Surgical and radiologic anatomy : SRA,1998,20(4).
22. Yu-Hang Zhu,Kai-Liang Cheng,Zhuan Zhong,You-Qiong Li,Qing-San Zhu. Morphologic evaluation of Chinese cervical endplate and uncinate process by three-dimensional computed tomography reconstructions for helping design cervical disc prosthesis[J]. Journal of the Chinese Medical Association,2016,79(9).
23. Kim Moon-Kyu,Kwak Dai-Soon,Park Chun-Kun,Park Se-Hyuck,Oh Sae-Moon,Lee Sang-Won,Han Seung-Ho. Quantitative anatomy of the endplate of the middle and lower cervical vertebrae in Koreans.[J]. Spine (Philadelphia, 1976),2007,32(14).
24. Dennis R. Osborne,Ralph E. Heinz,D. Bullard,A. Friedman. Role of Computed Tomography in the Radiological Evaluation of Painful Radiculopathy after Negative Myelography: Foraminal Neural Entrapment[J]. Neurosurgery,1984,14(2).
25. EPSTEIN J A,LAVINE L S,ARONSON H A,EPSTEIN B S. CERVICAL SPONDYLOTIC RADICULOPATHY. THE SYNDROME OF FORAMINAL CONSTRICTION TREATED BY FORAMENOTOMY AND THE REMOVAL OF OSTEOPHYTES.[J]. Clinical Orthopaedics and Related Research,1965,40.
26. TENG P. Spondylosis of the cervical spine with compression of the spinal cord and nerve roots. Journal of Bone & Joint Surgery American Volume,1960, 42-A(3), 392.
27. Shuaifeng Yan,Yunfan Zhang,Kai Wang,Yingchao Han,Kai Zhu,Fan He,Jun Tan,William B. Rodgers. Three-Dimensional Morphological Characteristics of Lower Lumbar Intervertebral Foramen with Age[J]. BioMed Research International,2018,2018.
28. Manohar M. Panjabi,Travis G. Maak,Paul C. Ivancic,Shigeki Ito. Dynamic Intervertebral Foramen Narrowing During Simulated Rear Impact[J]. Spine,2006,31(5).
29. Ebraheim N A,Lu J,Biyani A,Brown J A,Yeasting R A. Anatomic considerations for uncovertebral involvement in cervical spondylosis.[J]. Clinical orthopaedics and related research,1997(334).
30. Humphreys S C,Hodges S D,Patwardhan A,Eck J C,Covington L A,Sartori M. The natural history of the cervical foramen in symptomatic and asymptomatic individuals aged 20-60 years as measured by magnetic resonance imaging. A descriptive approach.[J]. Spine,1998,23(20).
31. Sohn Hong Moon,You Jae Won,Lee Jun Young. The relationship between disc degeneration and morphologic changes in the intervertebral foramen of the cervical spine: a cadaveric MRI and CT study.[J]. Journal of Korean Medical Science,2004,19(1).
32. Shin Yamazaki,Shoichi Kokubun,Yushin Ishii,Yasuhisa Tanaka. Courses of Cervical Disc Herniation Causing Myelopathy or Radiculopathy: An Analysis Based on Computed Tomographic Discograms[J]. Spine,2003,28(11).
33. Post NH, Cooper PR, Frempong-Boadu AK, Costa ME. Unique features of herniated discs at the cervicothoracic junction: clinical presentation, imaging, operative management, and outcome after anterior decompressive operation in 10 patients. Neurosurgery, 2006, 58(3), 497-501.
34. L PENNING,J T WILMINK. Rotation of the Cervical Spine: A CT Study in Normal Subjects[J]. Spine,1987,12(8).
35. John D. Clausen,Vijay K. Goel,Vincent C. Traynelis,Jeffrey Scifert. Uncinate processes and Luschka joints influence the biomechanics of the cervical spine: Quantification using a finite element model of the C5‐C6 segment[J]. Journal of Orthopaedic Research,1997,15(3).
36. Kotani Y,McNulty P S,Abumi K,Cunningham B W,Kaneda K,McAfee P C. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine. A biomechanical study.[J]. Spine,1998,23(14).
37. Snyder Joshua T,Tzermiadianos Michael N,Ghanayem Alexander J,Voronov Leonard I,Rinella Anthony,Dooris Andrew,Carandang Gerard,Renner Susan M,Havey Robert M,Patwardhan Avinash G. Effect of uncovertebral joint excision on the motion response of the cervical spine after total disc replacement.[J]. Spine (Philadelphia, 1976),2007,32(26).
38. Jung U. Yoo,Dewei Zou,W Thomas Edwards,James Bayley,Hansen A. Yuan. Effect of Cervical Spine Motion on the Neuroforaminal Dimensions of Human Cervical Spine[J]. Spine,1992,17(10).
39. Farmer JC1, Wisneski RJ. Cervical spine nerve root compression. an analysis of neuroforaminal pressures with varying head and arm positions. Spine, 1994, 19(16), 1850-1855.
40. Lee J-Y,Löhr M,Impekoven P,Koebke J,Ernestus R-I,Ebel H,Klug N. Small keyhole transuncal foraminotomy for unilateral cervical radiculopathy.[J]. Acta Neurochirurgica,2006,148(9).
41. Yilmazlar S,Ikiz I,Kocaeli H,Tekdemir I,Adim S B. Details of fibroligamentous structures in the cervical unco-vertebral region: an obscure corner.[J]. Surgical and Radiologic Anatomy,2003,25(1).
42. Macnab, I. The traction spur. Journal of Bone & Joint Surgery, 1971, 53(4), 663-670.
43. Sizer P S,Phelps V,Brismee J M. Differential diagnosis of local cervical syndrome versus cervical brachial syndrome.[J]. Pain Practice,2006,1(1).
44. Dvorák J. Epidemiology, physical examination, and neurodiagnostics.[J]. Spine,1999,23(24).
45. Paul Dreyfuss,Mark Michaelsen,David Fletcher. Atlanto-Occipital and Lateral Atlanto-Axial Joint Pain Patterns[J]. Spine,1994,19(10 Suppl).
46. Pesch H J,Bischoff W,Becker T,Seibold H. On the pathogenesis of spondylosis deformans and arthrosis uncovertebralis: comparative form-analytical radiological and statistical studies on lumbar and cervical vertebral bodies.[J]. Archives of Orthopaedic and Trauma Surgery,1984,103(3).
47. Brismée Jean-Michel,Sizer Phillip S,Dedrick Gregory S,Sawyer Barbara G,Smith Michael P. Immunohistochemical and histological study of human uncovertebral joints: a preliminary investigation.[J]. Spine (Philadelphia, 1976),2009,34(12).
48. Robert A. Robinson,George W. Smith. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome[J]. SAS Journal,2010,4(1).
49. Cloward Ralph B. The anterior approach for removal of ruptured cervical disks. 1958.[J]. Journal of Neurosurgery: Spine,2007,6(5).
50. Riley L H,Robinson R A,Johnson K A,Walker A E. The results of anterior interbody fusion of the cervical spine. Review of ninety-three consecutive cases.[J]. Journal of Neurosurgery,1969,30(2).
51. Bohlman HH1, Emery SE, Goodfellow DB, Jones PK.. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. long-term follow-up of one hundred and twenty-two patients. Journal of Bone & Joint Surgery American Volume, 1993, 75(9), 1298.
52. Craig D. Brigham,Paul J. Tsahakis. Anterior Cervical Foraminotomy and Fusion|Surgical Technique and Results[J]. Spine,1995,20(7).
53. Richard A. Davis. A long-term outcome study of 170 surgically treated patients with compressive cervical radiculopathy[J]. Surgical Neurology,1996,46(6).
54. Jho H D. Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation.[J]. Journal of neurosurgery,1996,84(2).
55. Connolly E S,Seymour R J,Adams J E. Clinical evaluation of anterior cervical fusion for degenerative cervical disc disease.[J]. Journal of Neurosurgery,1965,23(4).
56. Howard S. An,Christopher J. Evanich,Bruce H. Nowicki,Victor M. Haughton. Ideal Thickness of Smith—Robinson Graft for Anterior Cervical Fusion: A Cadaveric Study with Computed Tomographic Correlation[J]. Spine,1993,18(14 Suppl).
57. James C. Bayley,Jung U. Yoo,David M. Kruger,John Schlegel. The Role of Distraction in Improving the Space Available for the Cord in Cervical Spondylosis[J]. Spine,1995,20(7).
58. John G. Golfinos,Curtis A. Dickman,Joseph M. Zabramski,Volker K. H. Sonntag,Robert F. Spetzler. Repair of Vertebral Artery Injury During Anterior Cervical Decompression[J]. SPINE,1994,19(22 Suppl).
59. Peter Petty. Surgical Anatomy of the Anterior Cervical Spine: The Disc Space, Vertebral Artery, and Associated Bony Structures[J]. Neurosurgery,1997,41(1).
60. Shintani A, Zervas NT. Consequence of ligation of the vertebral artery. Journal of Neurosurgery, 1972, 36(4), 447-50.
61. Curylo L J,Mason H C,Bohlman H H,Yoo J U. Tortuous course of the vertebral artery and anterior cervical decompression: a cadaveric and clinical case study.[J]. Spine (Philadelphia, 1976),2000,25(22).
62. Milne N. The role of zygapophysial joint orientation and uncinate processes in controlling motion in the cervical spine.[J]. Journal of anatomy,1991,178.
63. Park Moon Soo,Moon Seong-Hwan,Kim Tae-Hwan,Oh Jae Keun,Jung Jae Kyun,Kim Hyung Joon,Riew K Daniel. Surgical Anatomy of the Uncinate Process and Transverse Foramen Determined by Computed Tomography.[J]. Global spine journal,2015,5(5).
64. Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct
65. Reina Yao,Stewart D. McLachlin,Parham Rasoulinejad,Kevin R. Gurr,Fawaz Siddiqi,Cynthia E. Dunning,Christopher S. Bailey. Influence of graft size on spinal instability with anterior cervical plate fixation following in vitro flexion-distraction injuries[J]. The Spine Journal,2016,16(4).
66. Chibbaro Salvatore,Makiese Orphee,Bresson Damien,Reiss Alisha,Poczos Pavel,George Bernard,Kemal Koc. Oblique Corpectomy to Manage Cervical Myeloradiculopathy[J]. Neurology Research International,2011,2011.
67. Kotani Y,McNulty P S,Abumi K,Cunningham B W,Kaneda K,McAfee P C. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine. A biomechanical study.[J]. Spine,1998,23(14).
68. Jing Chen,Jia Li,Gang Qiu,Jingchao Wei,Yanfen Qiu,Yonghui An,Yong Shen. Incidence and risk factors of axial symptoms after cervical disc arthroplasty: a minimum 5-year follow-up study[J]. Journal of Orthopaedic Surgery and Research,2016,11(1).
69. Jónsson H,Bring G,Rauschning W,Sahlstedt B. Hidden cervical spine injuries in traffic accident victims with skull fractures.[J]. Journal of spinal disorders,1991,4(3).
70. Yetkin Z,Osborn A G,Giles D S,Haughton V M. Uncovertebral and facet joint dislocations in cervical articular pillar fractures: CT evaluation.[J]. American Journal of Neuroradiology,1985,6(4).



 京公网安备11010502051256号
京公网安备11010502051256号